Abstract
Anterior crossbite is defined as a malocclusion characterized by the anterior maxillary teeth lingual position compared to mandibular anterior teeth. Anterior crossbite cases should be treated by emergency intervention in the early period to prevent problems such as abnormal enamel abrasion, periodontal pathologies, temporomandibular joint disorders, mobility, and fractures in teeth that may be caused by an anterior crossbite. In this case report, the treatment of 2 cases with anterior dental crossbite observed during the early mixed dentition period performed with different methods by considering their cooperation, personal characteristics, wishes, and needs is presented.
Introduction
Anterior crossbite can be clinically identified, when the anterior lower teeth are in a labial position regarding the anterior upper teeth.[1-3] Anterior dental crossbite has an incidence of 4-5%. It is usually observed in the early mixed dentition period and is caused by the abnormal eruption of permanent incisors.[4,5] This malocclusion may occur due to various factors such as a change in the position of the permanent tooth germ due to trauma to the primary incisors, delayed exfoliation of the primary incisors, supernumerary incisors, odontomas, crowding in the incisor region, and insufficient arch length.[4-6]
Anterior crossbite in the early mixed dentition period may have long-term adverse effects on the development and growth of teeth and jaws.[7] Anterior crossbite may lead to abrasion on the hard tissues of the tooth,[6,7] aesthetic problems, and asymmetries.[8] Furthermore, the mandibular incisors' proclamation may lead to the thinning of the labial alveolar crest and gingival recession.[8]
Case Presentation
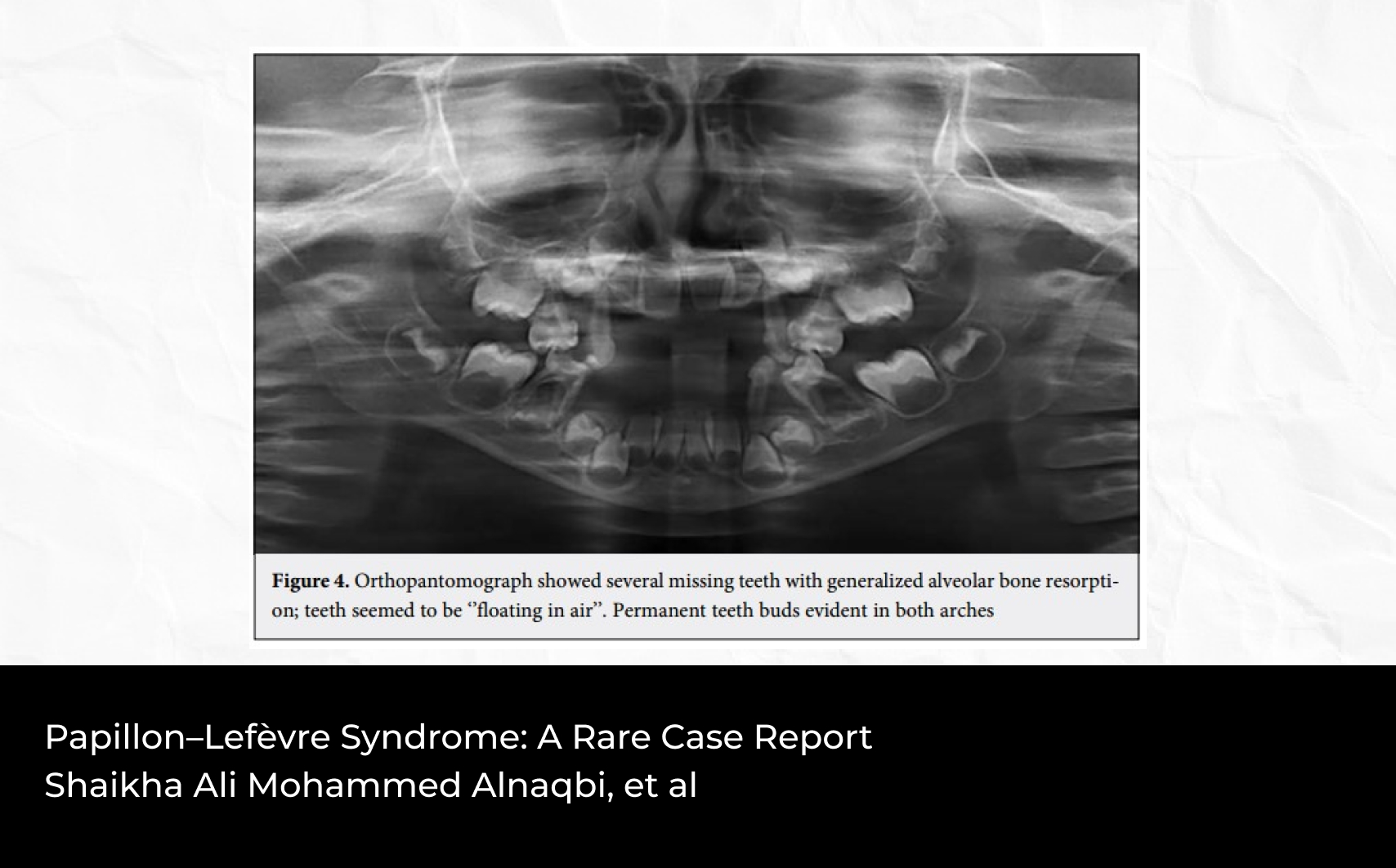
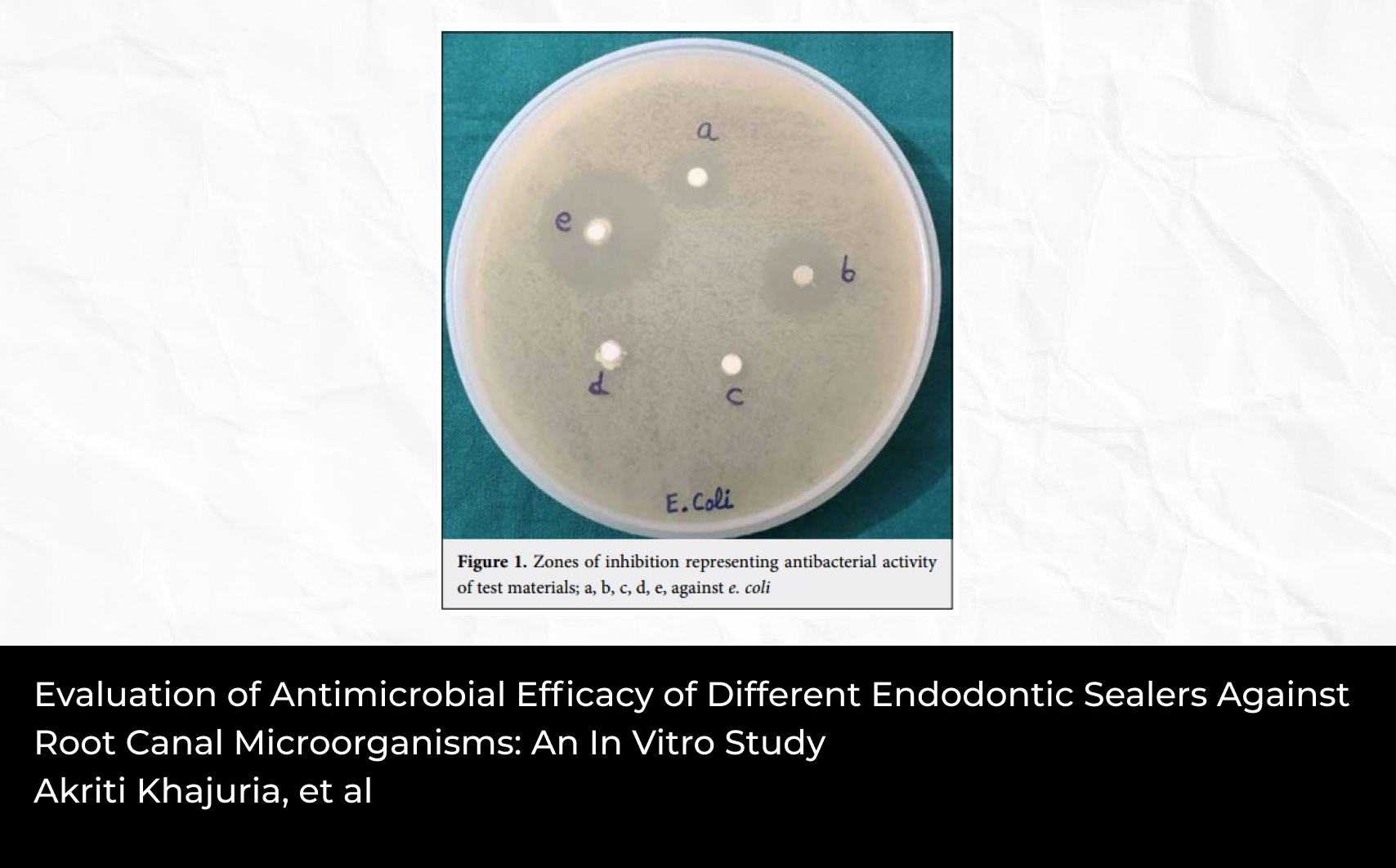
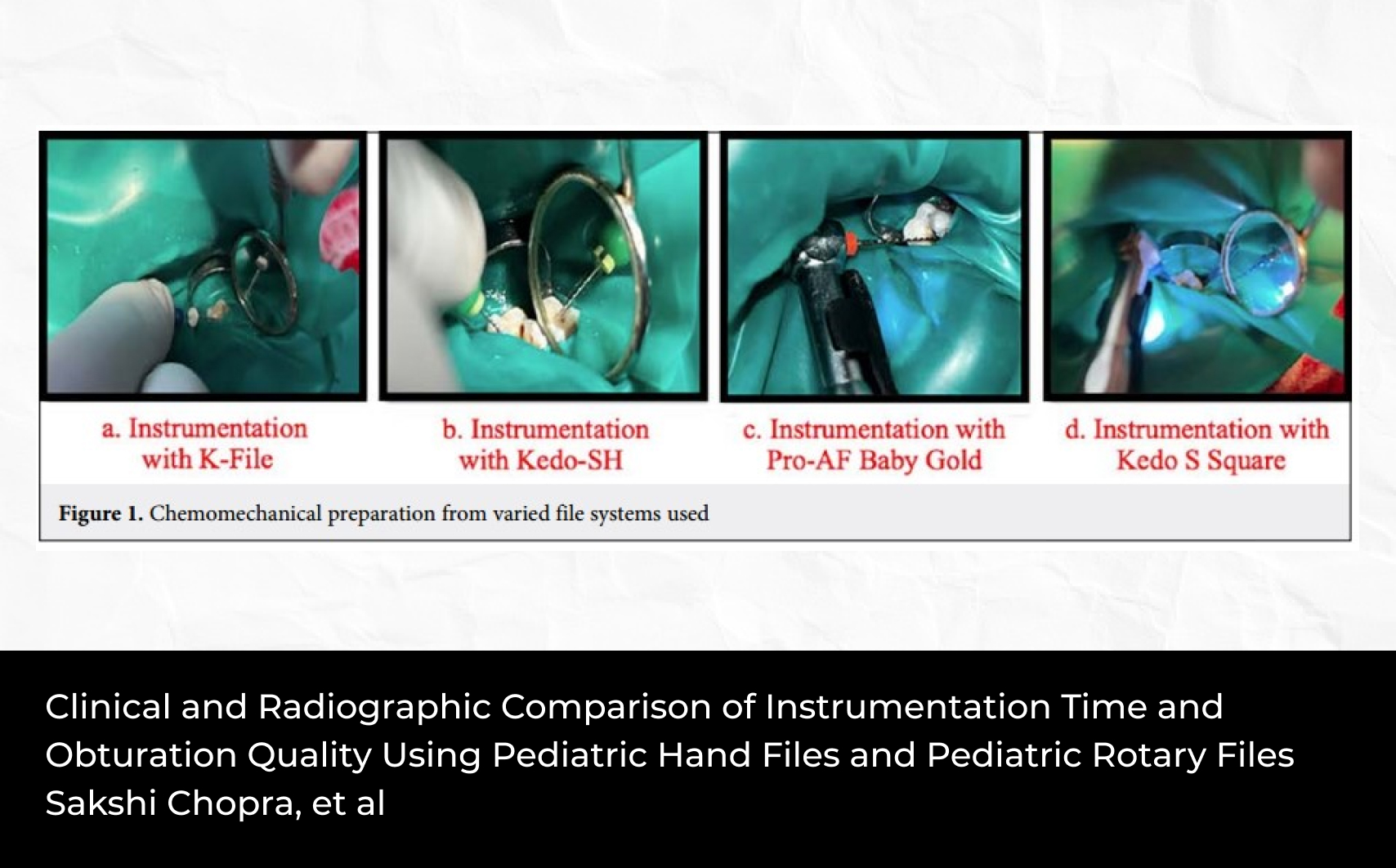
Case I: As a result of the intraoral examination of a 6-year-old girl admitted to our clinic with the complaint of crowding of her maxillary incisors, it was observed that anterior dental crossbite occurred due to palatally displaced left central incisor (Fig. 1). Furthermore, it was determined that the patient had mixed dentition and a Class I molar relationship. In the anamnesis, it was learned that removable orthodontic appliance therapy was initiated in another clinic one month ago; however, the child refused to use the removable orthodontic appliance. Therefore, a different treatment method was preferred. Compomer (Dyract, Dentsply, Konstanz, Germany) was placed on the occlusal surface of the mandibular primary molars, and bite-opening was performed in a balanced way with a distance of 2 mm between the incisal edges of the incisors (Fig. 2). The occlusal arrangement was made using articulating paper. After bite-opening was performed, abnormal contact between the upper left central tooth and mandibular incisors was eliminated (Fig. 3). Along with the tongue and lip's balanced pressure, the upper left central tooth was expected to be in the correct position. In control performed one month later, it was observed that the crossbite was successfully corrected. The compomer placed on the occlusal surface of the primary molars was removed. The treatment was terminated by restoring the occlusion to its previous state (Fig. 4).
Case II: In the general intraoral examination of a 6-year-old boy, it was observed that anterior dental crossbite occurred due to palatally displaced right central incisor (Fig. 5). Furthermore, it was determined that the patient had mixed dentition and a Class I molar relationship. In this case, a different treatment method was preferred because the parent did not want the removal of the fixed space maintainer in tooth number 55, the child was at a young age, and the use of the removable orthodontic appliance in the lower jaw was more difficult compared to the upper jaw. Resin modified glass ionomer cement (Fuji II LC Capsule, GC Corp., Tokyo, Japan) was placed on the occlusal surface of teeth 16, 65, and 26 to perform a balanced bite-opening with a distance of 2 mm between the incisal edges of the incisors. The decayed tooth number 64 was restored with compomer (Dyract, Dentsply, Konstanz, Germany), compomer (Dyract, Dentsply, Konstanz, Germany) was placed on the occlusal of tooth number 55 on which the space maintainer was previously placed, and the occlusal arrangement was made using articulating paper (Fig. 6). After bite-opening was performed, abnormal contact between the upper right central tooth and mandibular incisors was eliminated. Along with the tongue and lip's balanced pressure, the upper left central tooth was expected to be in the correct position. In control performed one month later, it was observed that the crossbite was successfully corrected. The restorative materials placed on the posterior teeth' occlusal surface were reduced to the normal occlusion position. In control performed after eight months, it was observed that there was no problem in the position of tooth number 11 (Fig. 7).
Discussion
Different techniques can be used in the treatment of anterior dental crossbite. The treatment aims to direct the affected maxillary incisors or teeth to the point where there will be a stable overjet-overbite relationship. Because normal overjet-overbite relationship prevents recurrence.[9] Hawley plates with active springs that increase occlusion can be used to treat anterior dental crossbite.[10] Significant results can be achieved in a short time with the composite inclined planes applied to the opposing tooth contacting with the maxillary teeth in crossbite.[11] Anterior dental crossbite can also be treated by placing a composite or compomer on the posterior teeth' occlusal surfaces and raising the occlusion.[12] Miamoto et al[13] stated that no significant differences were observed between the two protocols: use of a removable maxillary biteplate with finger springs and bonding of resin-reinforced glass ionomer cement bite pads on the lower first molars, for the correction of an anterior crossbite in the mixed dentition.
Anterior crossbite can be corrected with fixed treatments in adults since it may lead to functional problems.[14] The most important factors that ensure orthodontic treatment success are the physician's knowledge, experience, and skills; however, the desired results cannot be achieved unless the treatment is accompanied by patient compliance and parents' practical cooperation. A problem that may occur in patient compliance may negatively affect the ideal treatment plan and mechanics, extend the treatment length, and even make the treatment unsuccessful.[15-18] Different appliances are used in different individuals according to their problems and need to achieve the desired results during orthodontic treatment.[18] In both cases, we reported, a different treatment method that did not require children to use appliances was preferred by considering the cooperation, personal characteristics, wishes, and needs of the children. Bite-opening was performed in a balanced way by placing dental restorative materials on the posterior teeth' occlusal surface. In other words, the obstacle preventing the teeth from reaching their ideal position was eliminated, and treatment was performed. With this method preferred, although the patient's duration of sitting on the dental chair was extended, successful results were achieved with short-term treatment without the need for the appliance. In addition, a fixed appliance was more cost-effective than a removable appliance in the correction of an anterior crossbite with a functional shift.[19]
The most significant factor in this treatment's success was that the tooth in the crossbite was in the eruption phase. It is very easy for the teeth that have not entirely erupted to reach their ideal position.[20] If the obstacle that causes the crowded eruption of the teeth in the eruption phase can be eliminated, the tooth will spontaneously come to its position.
Conclusion
It is possible to prevent more severe malocclusions such as Class III anomalies and laterognathia that may occur in the future due to the simple treatment of anterior dental crossbite without skeletal asymmetry in mixed dentition.[21] Furthermore, the treatment method should be determined by considering the cooperation, personal characteristics, wishes, and needs of the patient.
Financial Disclosure: Nil.
Conflict of Interest: None declared.
References
1. Sollenius O, Petrén S, Bondemark L. An RCT on clinical effectiveness and cost analysis of correction of unilateral posterior crossbite with functional shift in specialist and general dentistry. Eur J Orthod 2020;42(1):44-51 doi:10.1093/ejo/cjz014
2. Asiry MA, AlShahrani I. Prevalence of malocclusion among school children of Southern Saudi Arabia. J Orthod Sci 2019;8:2. Published 2019 Feb 20 doi:10.4103/jos.JOS_83_18
3. Yu X, Zhang H, Sun L, Pan J, Liu Y, Chen L. Prevalence of malocclusion and occlusal traits in the early mixed dentition in Shanghai, China. PeerJ 2019;7:e6630 doi:10.7717/peerj.6630
4. Heikinheimo K, Salmi K, Myllärniemi S. Long term evaluation of orthodontic diagnoses made at the ages of 7 and 10 years. Eur J Orthod 1987;9(2):151-159 doi:10.1093/ejo/9.2.151
5. Hannuksela A, Väänänen A. Predisposing factors for malocclusion in 7-year-old children with special reference to atopic diseases. Am J Orthod Dentofacial Orthop 1987;92(4):299-303 doi:10.1016/0889-5406(87)90330-1
6. Bayrak S, Tunc ES. Treatment of anterior dental crossbite using bonded resin-composite slopes: Case reports. Eur J Dent 2008;2(4):303-306
7. McNamara JA Jr. Early intervention in the transverse dimension: is it worth the effort?. Am J Orthod Dentofacial Orthop 2002;121(6):572-574 doi:10.1067/mod.2002.124167
8. Valentine F, Howitt JW. Implications of early anterior crossbite correction. ASDC J Dent Child 1970;37(5):420-427
9. Croll TP. Fixed inclined plane correction of anterior cross bite of the primary dentition. J Pedod 1984;9(1):84-94
10. Estreia F, Almerich J, Gascon F. Interceptive correction of anterior crossbite. J Clin Pediatr Dent 1991;15(3):157-159
11. Sari S, Gokalp H, Aras S. Correction of anterior dental crossbite with composite as an inclined plane. Int J Paediatr Dent 2001;11(3):201-208 doi:10.1046/j.1365-263x.2001.00256.x
12. Tse CS. Correction of single-tooth anterior crossbite. J Clin Orthod 1997;31(3):188
13. Miamoto CB, Marques LS, Abreu LG, Paiva SM. Comparison of two early treatment protocols for anterior dental crossbite in the mixed dentition: A randomized trial. Angle Orthod 2018;88(2):144-150 doi:10.2319/052117-344.1
14. Brooks SA, Polk M. Anterior crossbite correction with fixed appliances in the adult dentition. Gen Dent 1999;47(3):298-300
15. Allan TK, Hodgson EW. The use of personality measurements as a determinant of patient cooperation in an orthodontic practice. Am J Orthod 1968;54(6):433-440 doi:10.1016/0002-9416(68)90198-x
16. Nanda RS, Kierl MJ. Prediction of cooperation in orthodontic treatment. Am J Orthod Dentofacial Orthop 1992;102(1):15-21 doi:10.1016/0889-5406(92)70010-8
17. Weiss J, Eiser HM. Psychological timing of orthodontic treatment. Am J Orthod 1977;72(2):198-204 doi:10.1016/0002-9416(77)90061-6
18. Ağar U, Doruk C, Babacan H, Bıçakçı A. Headgear kooperasyonunun değerlendirilmesinde hastalar ve velilerinin güvenilirliği. Cumhuriyet Dent J 2003;6(1):28-30
19. Khalaf K, Mando M. Removable appliances to correct anterior crossbites in the mixed dentition: a systematic review. Acta Odontol Scand 2020;78(2):118-125 doi:10.1080/00016357.2019.1657178
20. Doruk C, Göyenç Y. Ortodontik tedavilerde spontan diş hareketinin önemi. Cumhuriyet Dent J 2001;4(1):24-27
21. Uslu Ö, Toygar Memikoğlu TU. Treatment of anterior dental crossbite: A case report. ADO J Clin Sci 2007;1:43-46